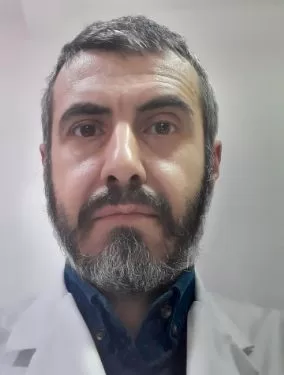
Persistent physical symptoms without an explicit cause, but which affect the quality of life of patients on most days, for months, are called somatization. Why do we somatize? Dr. Claudiu Ionescu, psychiatrist, doctor of medicine, university lecturer at the "Carol Davila" Faculty of Medicine and Pharmacy, Bucharest, offers us some explanations regarding this medical problem.
If you have questions about somatization and feel the need
to talk to a specialist, do not hesitate to schedule an online consultation
with one of the psychiatrists available on the Digital Clinics platform.
What is somatization?
The definition of somatization is based on the duration and
frequency of persistent symptoms and the suffering they induce, often
independently of the etiology of the symptoms. "Somatization is,
regardless of the cause, a symptom that can be found on its own, can be
persistent in certain somatic diseases, and can be individualized in the form
of functional somatic disorders or so-called psychosomatic diseases, such as
irritable bowel syndrome. Yes, irritable bowel syndrome most often has
psychoemotional causes," explains doctor Claudiu Ionescu.
How does it manifest itself?
Often, somatizations or somatic symptoms appear atypically,
without any medical explanation. In 50% of consultations, some studies say,
patients present with persistent somatic symptoms, whether it is abdominal
digestive symptoms, headaches, back pain, fatigue and others. "Half of the
patients may present these symptoms during primary care consultations, during
several changes of doctors, in order to finally reach the psychiatrist, who is
the most experienced and most knowledgeable in addressing these somatic
symptoms in a complex and complete way. Their burden correlates quite poorly
with the severity or stage of an underlying disease, which is why they are also
very late in diagnosis, somatic symptoms are often passed through several
filters by non-psychiatric doctors in order to finally reach a
psychiatrist," says Dr. Claudiu Ionescu.
Causes of somatization
The risk factors of somatic disorders are complex. They are
biological factors, psychological factors and psychosocial factors. They all
contribute to the onset and especially the persistence of somatic symptoms.
Sometimes they contribute individually, sometimes in combination. The most
influential are psychological and psychosocial factors, especially when we talk
about the persistence of somatization in the long term.
Profile of the patient with somatizations
Usually, the patient with somatizations or somatic causes is
a female patient, with a secondary education, who has experienced adverse,
psycho-stressful events in life, or the so-called stressors. "The person
has had untreated depressive or anxious episodes, various moments of negative
affectivity, perhaps they have had contact with people who had illnesses that
greatly affected their quality of life or who were in the terminal stage of the
disease, or they have been caregivers of such people. Epigenetic factors,
endocrine factors, microbiota predispositions that precipitate the onset of
somatic symptoms, which apparently have no explanation, can also
intervene", adds psychiatrist Claudiu Ionescu. To all these factors are
added trigger factors that can be acute infection-type factors, stressful life
events, psycho-shocking events, or they can also be factors that maintain and
worsen somatic symptoms. "This is where the frustration of patients and
doctors comes in, because everything seems to be under the same umbrella
generically called "it's all in your head!" That is, there are those
cognitive, perceptual and emotional factors, which involve a very focused
attention on interpretations of symptoms and a somato-sensory amplification,
which is called health anxiety. They are often accompanied by behavioral
responses such as excessive use of self-medication or informational contagion
via the Internet, meaning the patient looks for answers on the Internet, in
social media and in other groups."
The connection between physical symptoms and stress
Mental health specialists say that stress, which can lead to
the development of anxiety, initially only generates a series of responses to
adapt to new realities, represents a way to cope with pressure, to perform in
new conditions, generates an ancestral biological reaction of the fight, flight
or freeze type, therefore determines a defense reaction deeply embedded in our
limbic system, in the pituitary area, connected to the adrenal cortex area,
which once activated represents the maladaptive response to stress, which, in
the long term, can lead to a not very strong, but continuous discharge of
cortisol. This discharge, over time, leads to the well-known effects of stress
– increased heart rate, palpitations, gastric acidity, intestinal hyperactivity
or hypoactivity, muscle tension that can cause headaches, back pain, autonomic
vegetative hyperactivity, sensations of dizziness, sweating, tremors, and these
for doctors who observe them for the first time seem inexplicable. "All
these sensations are all a fight-or-flight reaction and constitute a
hyperactivation of maladaptive stress responses. The stress may pass, but the
body remains on this alert. This can lead to the so-called somatosensory
amplification phenomenon, given by symptoms that are already in the body such
as palpitations, belching, epigastric pain, tremors, sweating. ", explains
doctor Ionescu.
Specialists talk about the predictive coding model, which
means that, based on past perceptual experiences, our brain ends up coding the
body's reactions and the signals that come from the body in a certain way, and
in order not to make mistakes in the predictions it makes, it also integrates
maladaptive signals such as somatic symptoms. And then the somatic symptoms are
maintained and worsen because the predictive coding model tells us that, in
fact, the brain begins to maintain them based on this learning as if they were
real again.